Why Gut Protocols Fail
My before-and-after stool tests revealed a hard truth: you can’t kill your way to balance. Here’s what really works.
I’ve always told people: if you’re working on your gut, you have to retest.
One stool test gives you a snapshot, but without a follow-up, you have no idea if your protocol actually worked, or if it just shifted things around.
So, I followed my own advice.
I ran a 4-week gut protocol. Then I retested.
And just like I’ve been saying for years, the results didn’t show a neat “all-clear.” Some pathogens were gone, some were reduced, and others actually increased. That’s the reality of gut protocols: a short phase isn’t usually enough, and without retesting, you’re flying blind.
First, I’m already healthy
This is important to understand up front: I already consider myself to be very healthy.
I get >2 hours of deep sleep every night.
My HRV sits solidly between 80–100.
I’m making progress in the gym consistently.
I tan easily and evenly without burning or getting sunspots, compared to the past.
My motivation, drive, and life aggression are high.
My bloodwork is excellent.
I have clear skin, no hair loss, crystal-clear vision.
In other words, I wasn’t chasing this stool test because I felt broken. I was chasing it because I’m obsessed with optimization, taking health from great to elite.
The gut protocol & die-off
For reference, I’m doing the GI map with SCFA and bile addon test.
After seeing some (quite severe) overgrowth in pathogens, I was quite shocked, but then created a comprehensive gut protocol of anti-microbials to blast them all into kingdom come.
I chose specific anti-microbials to target the specific bacteria, not just a random shotgun approach.
When I started my 4-week gut protocol, I almost immediately noticed die-off symptoms.
My deep sleep dropped from 2 hours down to <1 hour on alternating nights.
I developed huge inflammatory bacne.
My feet became extremely smelly.
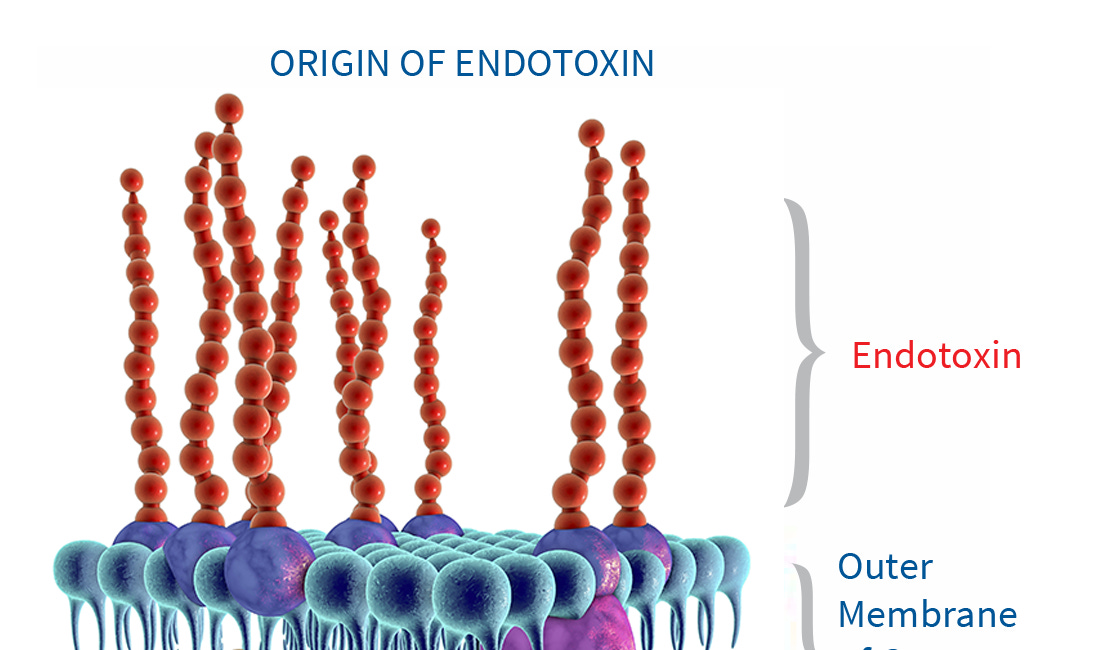
These are all classic signs of microbial die-off and inflammatory endotoxin release. The good news? After about 2 weeks, those symptoms cleared, and my sleep rebounded.
That alone told me something real was happening in the gut, but I wanted the data. I also think that the reason my die off was so mild is because I was using a lot of anti-inflammatories and binders, to prevent the endotoxin and other toxins to inflame me and enter into the body.
What Changed After 4 Weeks
Honestly, I thought my protocol was overkill and I would wipe out all those MFers for good. But turns out I wasn’t so lucky.
When I compared my two stool tests side by side, the data told a nuanced story. Some pathogens were cleared, some improved dramatically, but others either persisted or grew stronger. This is exactly why I tell people: a gut protocol without retesting is just guessing.
What improved
The good news: the protocol absolutely worked in key areas.
Pathogens cleared completely:
Before the protocol, my test flagged EHEC and its two shiga toxins (stx1, stx2) at high levels. Four weeks later, all of them were completely undetectable. Candida also normalized to “not detected.”Opportunists knocked down hard (but still too high):
Pseudomonas went from borderline high (1.01e4) to comfortably normal (3.76e2).
Staphylococcus spp dropped from 1.15e5 to below detection, while S. aureus itself halved from 1.35e4 → 7.49e3.
Enterococcus species like E. faecalis and E. faecium also plummeted by 84–94%.Commensals trending upward:
Some of my beneficial bacteria rebounded:Lactobacillus spp doubled, climbing from 42% → 86% of the reference range.
Bacteroides fragilis nearly quadrupled (6% → 27% of range).
Roseburia (a butyrate producer) shot up ~9×, reaching almost 50% of the healthy range.
Even Faecalibacterium prausnitzii, an important anti-inflammatory butyrate-producing species, increased ~9×, though it still sits far below optimal.
Immune defense rebounded:
Secretory IgA rose from a low 323 to a healthy 1446, showing my mucosal immune system is much more active and responsive now.
Together, these changes confirm the protocol wasn’t wasted effort. It had clear wins: pathogens removed, overgrowths suppressed, beneficials nudging upward, and immune tone restored.
What didn’t improve
But here’s the catch, not everything moved in the right direction.
Opportunists filled the gap:
Citrobacter exploded from 3.06e5 → 2.05e6 (~7× increase).
Enterobacter went nuclear, jumping from 1.75e4 → 5.11e6 (~292× increase).
Fusobacterium also bloomed from 2.83e3 → 2.12e5 (~75× increase).
This is a classic case of “kill some, others expand” — opportunists seizing the vacant niches.
Commensals collapsed:
My commensal E. coli crashed from a robust 3.39e9 (top of the healthy range) down to 2.16e5 (barely detectable).
Akkermansia muciniphila, a keystone mucus-protecting bacterium, dropped ~95% and fell below the reference range.
Some overgrowths persisted:
While E. faecalis and E. faecium dropped, the genus Enterococcus overall is still massively elevated (2.07e8 vs ref <1.0e5).
Staphylococcus aureus improved but remains above reference.
Why these pathogens are “bad”
1. Enterobacter + Citrobacter
Endotoxin factories: Both are gram-negative Enterobacteriaceae, so they produce lipopolysaccharide (LPS), one of the most potent endotoxins in the body.
Impact: LPS increases intestinal permeability (“leaky gut”), activates TLR4 (endotoxin receptor) on immune cells, drives cytokine release (inflammation), and loads the liver with detox work. Chronically, this can lower testosterone, increase insulin resistance, and contribute to fatigue and mood issues.
2. Fusobacterium
Inflammatory niche: Fusobacteria are linked with colonic inflammation and even colorectal cancer risk when elevated.
Mechanism: They adhere tightly to gut lining, disrupt tight junctions, and promote a local inflammatory environment. They’re also associated with butyrate depletion, which means they compete against beneficial SCFA producers like Roseburia and Faecalibacterium.
3. Staphylococcus aureus (and high Staph spp)
Toxin producers: S. aureus can release enterotoxins that trigger gut inflammation and food poisoning-like symptoms.
Barrier stress: They don’t just cause acute illness, they also stress the mucosal immune system (your IgA spike is partly a response to them).
4. Enterococcus spp (high genus signal)
Opportunists: While they can be part of a “normal” microbiome, when elevated, they produce biogenic amines and secondary bile salt hydrolases that irritate the gut lining.
Clinical context: Overgrowth is often linked to hospital infections (antibiotic resistance), but even subclinical elevations can push systemic inflammation.
The unifying problem: endotoxin & inflammation
Most of these species (especially Enterobacter, Citrobacter, Fusobacterium) cause issues not just by “being there,” but by what they produce:
Endotoxins (LPS): Trigger systemic inflammation, liver stress, and hormonal disruption.
Toxins/exotoxins: Staph and Enterococcus secrete compounds that irritate gut tissue.
Competition: They crowd out commensals like E. coli and Akkermansia, further weakening your barrier.
The main danger is endotoxin overload → leaky gut → liver detox burden → systemic inflammation.
The lesson
This is the reality of gut protocols: you don’t get a clean slate in 4 weeks or even after 1 gut protocol. You knock some down, others rebound, and new players emerge. Without retesting, I’d never know Citrobacter, Enterobacter, and Fusobacterium were now the main threats and I might have assumed the job was “done.”
But the truth is, gut healing isn’t a one-and-done kill phase. It’s kill, rebuild, retest, adapt. That’s the cycle. My results proved it, and it’s why I’ll always retest and refine and why I tell everyone else to do the same.
The takeaway → what’s next
The big lesson here is simple: gut protocols are not one-and-done. Without retesting, I would never have seen that shift.
In hindsight, I could have paired my antimicrobial stack with fiber-based prebiotics. That might have promoted a faster bloom of beneficial strains and prevented opportunists from rushing into the empty space. It’s a reminder that competition is the real game in the gut; when one group is knocked down, something else will always try to fill the vacuum.
That’s why I’m continuing the process, not stopping here. My next experiments are mapped out and precise.
And of course, I’ll be retesting my stool after each phase. That’s how you know whether your interventions are working, not by guesswork, but by data.
👉 The moral of the story: kill, rebuild, retest, adapt. That’s the only way to make gut healing stick long-term.
And here’s the last point: it’s important not to just keep slamming antimicrobials. They’re powerful, but they don’t discriminate. Overuse can wipe out your allies too, as I saw with my commensal E. coli and Akkermansia, both of which dropped hard. Gut health is about balance, not total annihilation.
What if you can’t test right now?
Not everyone can run a stool test every 4–8 weeks. That’s fine.
If that’s you, then start with the principles I laid out in my Lowering Endotoxin article:
Use specific prebiotics and probiotics to favor SCFA-producers and keep pathogens in check.
Improve transit time so endotoxin doesn’t accumulate.
Seal the gut barrier to minimize endotoxin absorption.
Bind endotoxin so it can be carried out rather than reabsorbed.
If you follow those steps consistently, you can gradually lower pathogenic overgrowth and blunt almost all of the damage endotoxin causes, even without testing.
That’s exactly how I’ve stayed extremely healthy with great labs, high energy, and strong performance, even while my stool tests still show some opportunists present. The difference is, I knew what to do to keep the effects under control.


Maybe do a before and after test with raw milk diet as prescribed by dr porter?