A high LH often always means poor LH receptor sensitivity at the Leydig cells.
Quick intro to steroidogenesis
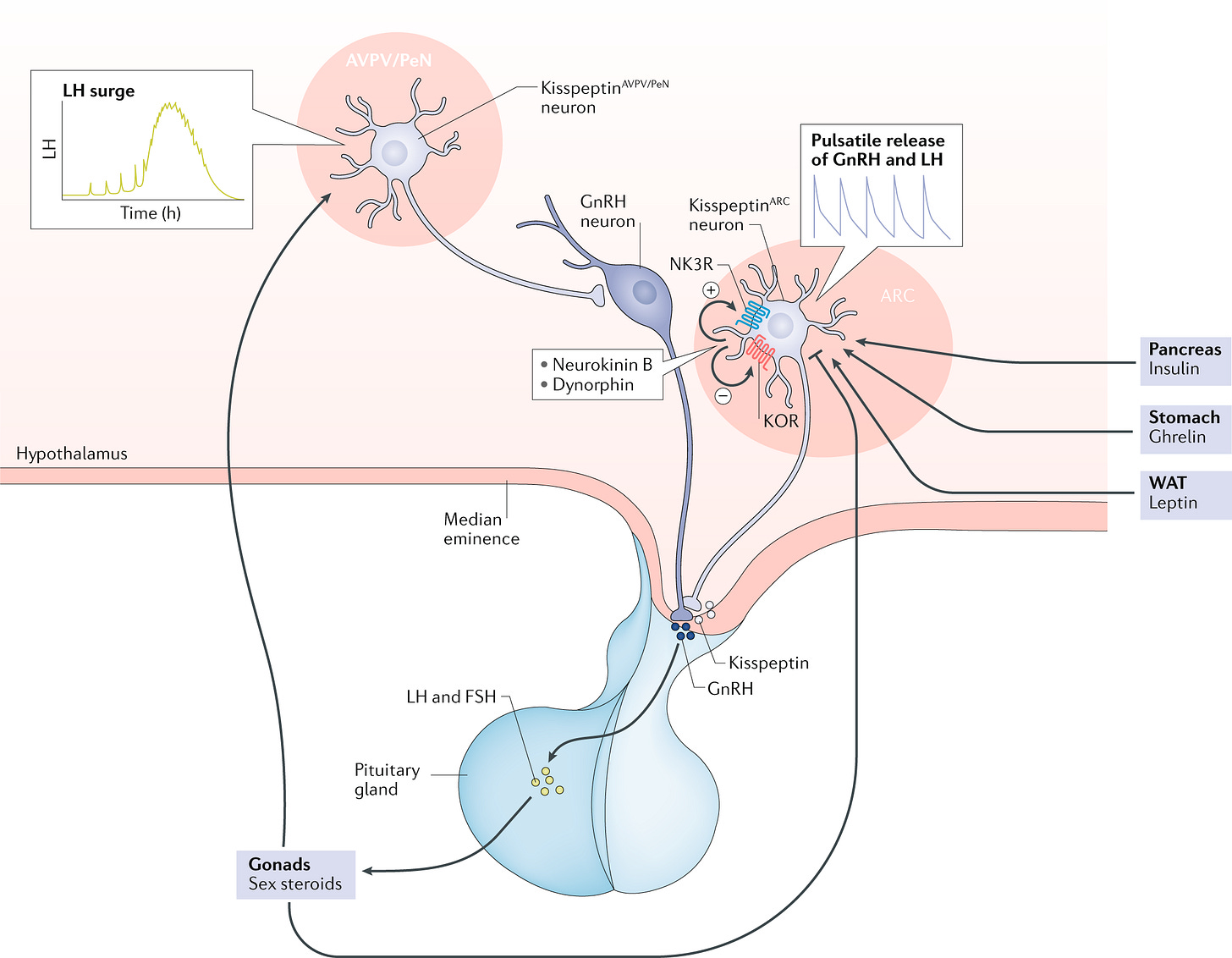
Steroidogenesis begins in the hypothalamus with the release of kisspeptin, which acts as a master switch for reproductive hormone signaling. Kisspeptin stimulates the secretion of GnRH (gonadotropin-releasing hormone) in a pulsatile manner, which then signals the anterior pituitary gland to release LH (luteinizing hormone) and FSH (follicle-stimulating hormone).
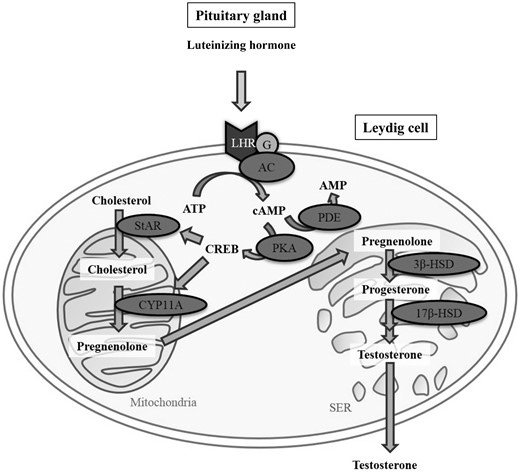
LH primarily targets the Leydig cells in the testes, where it activates the cAMP-PKA pathway, leading to the transport of cholesterol into mitochondria via the StAR protein—a key step that initiates steroid hormone production.
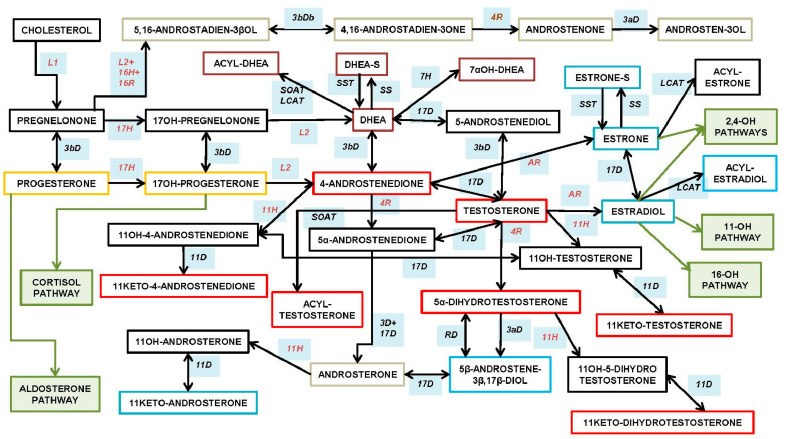
Inside the Leydig cells, cholesterol is converted into pregnenolone by the mitochondrial enzyme CYP11A1. This marks the start of true biochemical steroidogenesis. Pregnenolone is then enzymatically converted through a series of steps into progesterone, 17-OH-progesterone, and ultimately into androstenedione, which is further converted into testosterone via 17β-HSD.
Testosterone can then either act directly, be converted into the more potent DHT (dihydrotestosterone) by 5α-reductase, or be aromatized into estradiol by aromatase.
The LH receptor can either be reduced in amount (but remain sensitive) or become desensitized (while the amount remains the same), or both.
LH to testosterone ratio
The optimal range for LH (Luteinizing Hormone) is typically between 4 and 7 IU/mL.
If LH is below 4, the issue often originates at the hypothalamus or pituitary, indicating a central problem with hormone signaling.
If LH is above 7, it may reflect testicular insensitivity—where the Leydig cells aren’t responding effectively to LH stimulation.
There are also external influences that can skew LH levels:
Low LH may result from the use of HCG or TRT, which suppresses endogenous LH via negative feedback.
High LH may be caused by drugs like Clomid or Enclomiphene, which artificially boost GnRH and LH.
I’ve reviewed labs where a guy had total testosterone around 1000 ng/dL, LH at 3.5, and free T in the upper normal range. That suggests excellent Leydig cell sensitivity—his body is producing strong testosterone output with relatively low LH stimulation.
On the flip side, I’ve seen men with LH at 8 IU/mL and testosterone around 400 ng/dL—a clear sign of poor Leydig cell sensitivity.
The goal depends on what’s off:
If LH is low, the priority is to increase LH production.
If LH is high but testosterone is low, the focus should shift to improving testicular responsiveness to LH.
One last point to consider: if total T is high, LH is normal, but free T is low due to elevated SHBG, this doesn’t reflect optimal function either. In that case, the strategy should be to lower SHBG while also nudging LH higher to support free T levels.
What’s the point of injecting 250-500IU of HCG every other day or even daily and your T only goes to 500ng/dl.
Or you take 25mg of enclomiphene daily, and your LH spikes to 20, but your T is only around 600-700ng/dl.